Rethinking primary care beyond telemedicine
Why now is the time to innovate in healthcare and how design can help.
Covid-19 health crisis exposed the shortcomings of several health systems and made us question our current healthcare practices. In Italy, for example, the infection took off in health facilities; now experts and pundits are calling for full adoption of telemedicine. In this article I will argue that telemedicine only is not enough to make health systems stronger once we go back to normal. We need to look at the bigger picture of primary care. Regions in Italy with stronger primary care are proving to be able to handle epidemics better too, as it is crucial to assist patients in their community in order to avoid hospital congestion. These times are ripe for change, but we need to adopt a systemic approach to innovation.
What is primary care?
Primary care services provide the first point of contact in a healthcare system.
Its services work towards prevention, health education and promotion, treatment of acute as well as chronic illnesses. Primary care also provides coordination for the patient in complex cases. These are key services to ensure a healthy population. The aging population coupled with the rise of chronic illnesses make the ‘hospital model’ obsolete and unsustainable for health systems. As we need to shift our focus on prevention we must understand and unlock the benefits of primary care. Good primary care deals with 95% of all issues, improves the patient satisfaction and reduces costs on health systems as fewer people need to visit hospitals or emergency departments. A health system that is not primary care-led is a weak and expensive one.
The domain of primary care is broad and it is delivered by different figures: nurses, pharmacists, dentists, optometrists and, above all, general practitioners. As its services need to be delivered within the community, it could be said that primary care is really patient-centric.
The role of the General Practitioner
In several health systems in Europe, the general practitioner (GP) has the following roles:
- Provider of personalized care in terms of evaluation and prevention
- Gatekeeper of access to secondary care through prescriptions
- Advocate for the patient in navigating the health system
- Enabler of patient knowledge and self-management
GPs should be empathic listeners and good communicators. On the other hand, patients need to become active partners in managing their own health. In this relationship, GPs should have a key role in this empowerment process.
In an ideal world, the general practitioner is the backbone of the patient-healthcare relationship. However, the reality is very different. Current workloads do not allow for any of that. In Italy, there are 88 GPs per 100 thousand inhabitants, which means that some GPs have more than 1500 patients when the optimal doctor-to-patient ratio should be around 1:1000.
These conditions cripple the value that primary care delivers. If you have too many patients you fail to fulfill two key aspects: easy availability and trust relationship. There are two straightforward solutions to this:
- Get more medicine students to become GPs
- Involve more technology to reduce the workload on GPs
While solution #1 is difficult to achieve, solution #2 seems easier but we should not underestimate the effort required. You can’t just replace a real doctor visit with a video chat. First off, any telemedicine service needs to be integrated within the health system. GP at hand in the UK taught us a lesson on the importance of implementation. The second evidence comes from the tepid user adoption rate. Digital transformation in healthcare hasn’t even started when compared with the disruption seen in other industries. Why don’t people love telemedicine solutions as much as Spotify? There are a number of reasons but the most important, as obvious as it sounds: current solutions are not designed around user needs.
The current state of telemedicine
- I book a 10 minutes appointment with a random doctor
- I explain my health issues to a complete stranger
- I get a prescription or I get told I need a real visit with a doctor.
Is this what people really want? This experience has three main flaws:
- The scope is limited. I can only use it for a couple of dozen conditions
- The video medium is not very effective: Can you actually check my back pain?
- There is no patient-doctor relationship at all. Primary care has always come from locally trusted sources.
On top of this, there is the integration side too which I will not delve into for the sake of brevity. I am only going to say that after those 3 flaws are fixed, this experience makes sense only if it’s fully integrated with an electronic health record that is shared and accessible by other doctors and nurses.
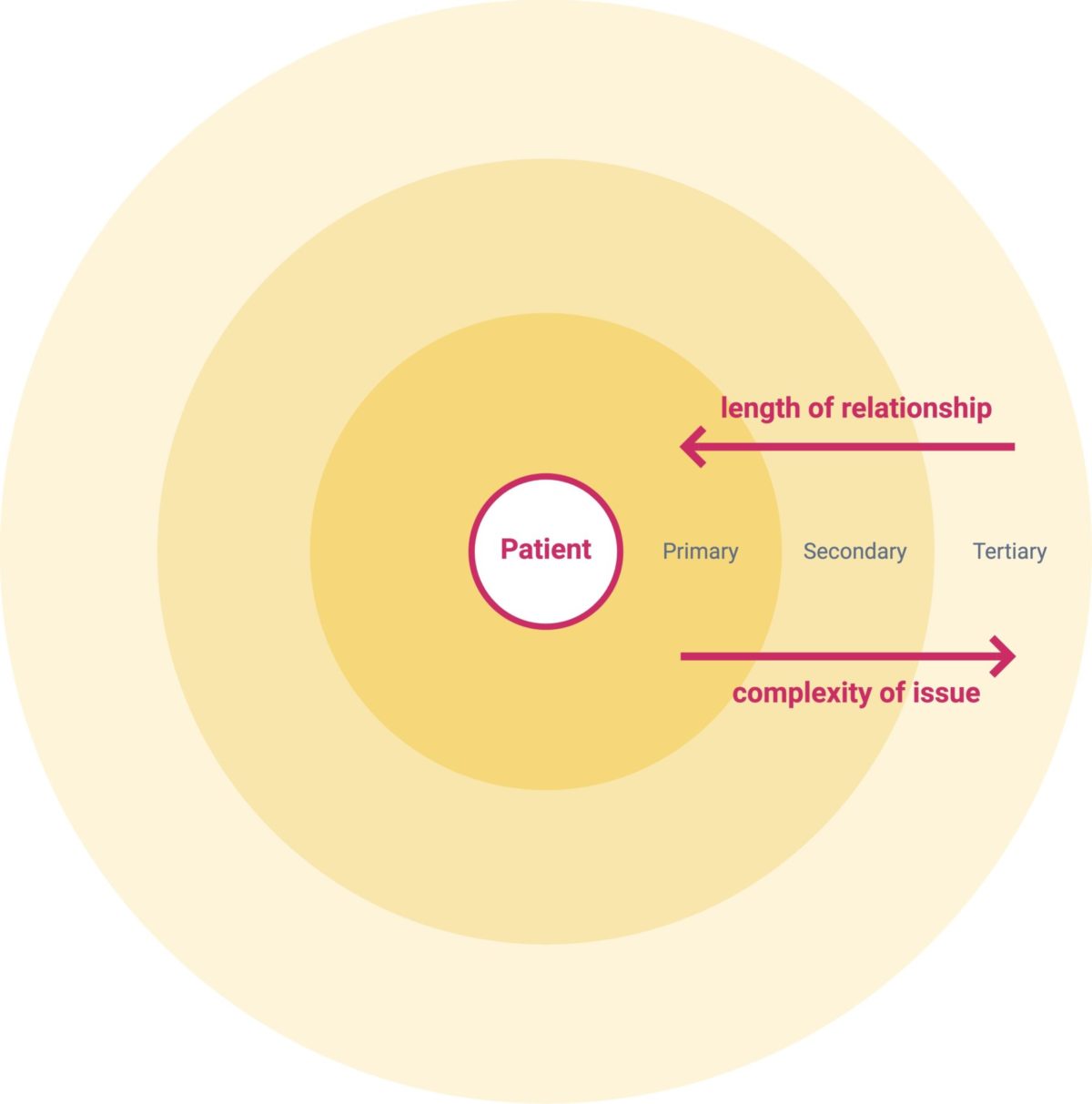
The current state of telemedicine comes from an approach that prioritizes what it can be built rather than what it should be built. Healthcare is a difficult ground and these are easy solutions that avoid facing complexity. In order to boost the adoption rate we should ditch the one-size-fits-all model and start to take into account different needs and preferences.
Lay the foundations
How might we design around those needs? I don’t have an answer in my pocket. I know we should start with people to rethink primary care delivery models that make good use of telemedicine. Pandemics aside, in normal times there are 4 main use cases for primary care. There are actually a lot more but let’s focus on the building blocks. Each use case is associated with a different need, therefore in each case, the person approaches healthcare with a different mindset. Each mindset should match with the right experience, which can be described by three key variables:
- The focus of the relationship between patient and healthcare
- The nature of the issue being treated
- The availability over time of this relationship
Use case 1:
I have a sudden acute need so I want quick advice on what I should do and maybe get a prescription.
Mindset:
These are symptoms common to many diseases but they appeared fairly quickly. I’m not that worried, they might go away in a while. It’s kind of urgent but I have work to do and I can’t be bothered to go to get an appointment, I’m looking for a convenient way to get advice. Even better If that’s available immediately.
Use case 2:
I need to do a routine check-up or a lab test I have been planning to do for a while.
Mindset:
I’ve been needing blood tests for a while. My doctor recommended them but it’s one of those things that I always forget to do. I’m feeling good anyway. I just don’t have much free time and I’m never close to one of those testing labs. Also, I probably need a prescription, right? If only the place was next to my office and there would be no waiting times.
Use case 3:
I broke my leg and I need someone who guides me through therapies and specialists.
Mindset:
I hurt myself at home, at the A&E they told me it’s broken and I will need physical therapy. Now what? I have seen 2 different radiologists and 1 therapist but I’m not sure I understand what they told me. When will I be able to go back to work? One doctor told me I should do therapy at home the other said it doesn’t matter. What should I do?
Use case 4:
I have a chronic condition I self-manage and I need to check in with someone who knows me
Mindset:
I’ve been living with this for years so I had to learn how to deal with it on a daily basis. Sometimes I want some that helps me cope with it but someone who actually understands what I’m going through. I also need to check in with the dosage of my meds regularly. I noticed this thing for a while. Do you think that’s good?
Editor’s note: Fictional scenarios, based on many real stories our designers have witnessed.
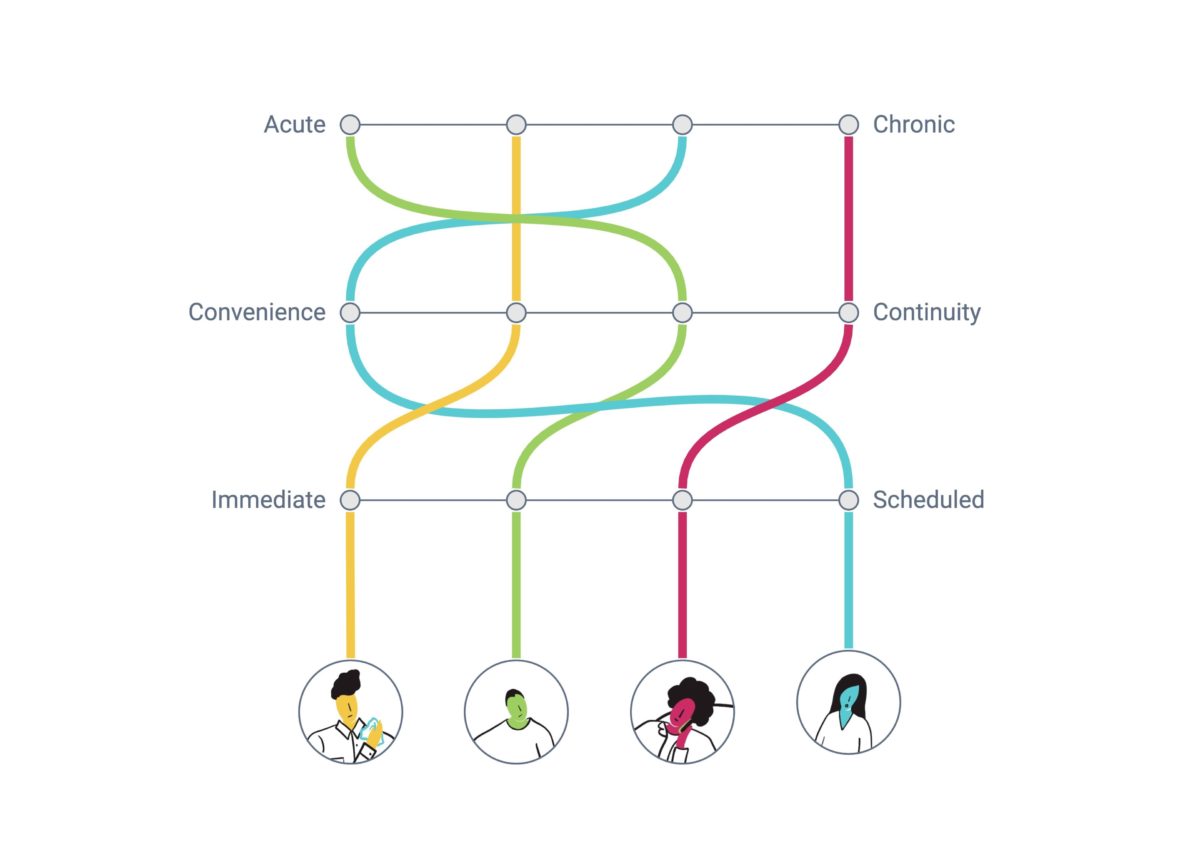
Easy, right? At first glance these four use cases make sense but the point is that experiences don’t happen in a vacuum. What happens if there is a pattern of use case 1 and I start noticing something might be off? Does that mindset still hold true? Chances are my needs change and I might prefer to talk to the same doctor. Then the question is whether that’s reasonable from a medical point of view. Is that feasible for the business? Let’s consider use case 4: how do I learn to self manage my chronic disease? What would the onboarding process look like? Do I get to choose a doctor that fits my clinical situation? About use case 2: How does my mindset change if I’m over 60 and I have an existing condition?
Conclusion
Covid-19 broke the status quo. Now is the time to change the paradigm and bring digital transformation to healthcare. Innovators should seize this opportunity now that the industry inertia has been put aside. Impactful solutions need to be human-centered and designers must go out in the field to study people. On top of that, we should facilitate and negotiate requirements with other disciplines. Healthcare is tough and the only way to tackle its problems is by making it a team sport.